Difference between revisions of "Open Source Medicine"
| Line 19: | Line 19: | ||
<big>"There is no medicine like hope, no incentive so great, and no tonic so powerful as expectation of something better tomorrow"</big> | <big>"There is no medicine like hope, no incentive so great, and no tonic so powerful as expectation of something better tomorrow"</big> | ||
<div style="text-align: right;">- Orison Swett Marden</div> | <div style="text-align: right;">- Orison Swett Marden</div> | ||
| − | {{ | + | {{frame more1|New treatments}}</div> |
| − | </div> | + | |
{{portalpageend}} | {{portalpageend}} | ||
Revision as of 18:47, 20 May 2010
|
Two key principles of this wiki are advanced automation and open collaboration. This page explores the application of these to healthcare, looking at how artificial intelligence can help automate healthcare and open collaboration can provide a more effective translation of knowledge into actual patient care. The medical systems now in existence are fraught with problems. The enormous amounts of data they gather remain disconnected and scattered, doctors are completely overwhelmed, much research (especially pharmaceutical) is done by private companies who take decades to develop drugs, and an unnecessary scarcity of healthcare lifts it out of the reach of the poor There is a way out: open source medicine and advanced automation. Use modern information technology to make medical knowledge freely available and share it globally by a standardized system. Develop drugs openly, so that people can pursue the research that matters to them, rather than base it on bottom-line considerations. Organize the medical knowledge of humanity intelligently and put it at the fingertips of every doctor. Automate as much of the medical system as possible (but no more!) to take the strain off doctors.
Keywords:
This page explores the application of automated information technology to healthcare, looking at how artificial intelligence can help automate healthcare and open collaboration can provide a more effective translation of knowledge into actual patient care. The medical systems now in existence are fraught with problems. The enormous amounts of data gathered remains disconnected and scattered. Doctors are completely overwhelmed. Cancer and heart disease are on the rise in rich countries, while in poor countries infectious diseases like AIDS storm on unabated. Much research (especially pharmaceutical) is done by private companies who take decades to develop drugs, and are more interested in baldness than in malaria. An unnecessary scarcity of proper healthcare lifts it out of the reach of the poor. A single solution can simultaneously make healthcare provided to the well-off more effective and make healthcare accessible to the poor. This solution is information-rich, open medicine. By properly integrating information revolution technology into our healthcare system, we can provide, at little or no cost to the user, a healthcare system more effective than anything we have imagined. We can switch from a system where medical treatment depends on scarce expertise and drugs to a system where it depends on ubiquitous information. Information-rich medicineThere are three elements in an information-rich medical system, all of which are greatly empowered by information technology: information must be gathered, processed, and communicated. These are explored in greater detail below. There are compelling reasons for setting up this information infrastructure according to open-source principles, where the platform and its content are built collaboratively, rather than being in the hands of a particular institution. Gathering informationWe have new, exponentially accelerating, ways of gathering medical and biological information. Traditionally, a doctor made clinical decisions based on the patient's descriptions of their symptoms and perhaps a few tests or low-resolution scans. But the body is a very complex thing, and this information gives only a very grainy picture of what is really happening. Several recently developed technologies allow us to gather literally millions of times more information about what's really going on in the body than was possible a few years ago -
These are the enabling tools of information-rich medicine. Using them in concert, you can build up a highly-detailed computerized set of information about what is going on with your body. Of course, to use the data effectively, it must be processed. Processing informationThis river of raw data would do a doctor no good; it would simply be overwhelming. This is where the pattern-recognition abilities of artificial intelligence are required. In the same way that artificial intelligence can recognize patterns showing a coming upswing in a stock market, it can recognize patterns in a heart rhythm indicating a coming heart attack. By applying A.I. to the data generated, we can turn raw data into clinically-relevant knowledge. This is already common practice in hospitals, where A.I. is routinely used for tasks like analyzing electrocardiograms. But can modern artificial intelligence really diagnose disease as effectively as human doctors? The surprising answer is that even mid-1970s artificial intelligence could. In the 1970s, an A.I. called MYCIN proved itself able to perform medical diagnosis as well as, or better than, human doctors. A patient can even do much of this processing on his or her smartphone. Smartphones can do blood glucose analysis, reconstruct ultrasound images and read and diagnose ECGs. Tasks demanding more computing power will require distributed cloud computing. One application of this is rational drug design, where A.I. considers the molecular basis of disease and computes the exact molecular intervention that is needed. This is a vast improvement on the old way of designing drugs based on chemical families. Even if the sophisticated information-gathering methods just described are not fully exploited, using existing artificial intelligence to process clinical information can greatly improve clinical outcomes. Imagine for a moment that if you walk into a clinic, modern information technologies whirr into action and pull from a distributed global network your medical record and family history. You describe your symptoms to the doctor, who inputs them into a handheld computer. The computer processes the symptoms and cross-references them with a database of known diseases. It compares all similarly-presenting cases – no matter where in the world those other cases happened. It uses all this information to create a list of possible diagnoses, then uses optimized and self-improving artificial intelligence algorithms to calculate the likelihood of each one, based on your medical history, race, age, sex and so forth. The computer displays a list of possible conditions and possible courses of action, including treatments or further testing. If a scan is done, say an X-ray, the computer can identify patterns in it and use this to inform its diagnosis. Such a system would never overlook a piece of data such as a drug interaction or allergy, and could intelligently update itself based on the entirety of mankind's medical knowledge. Add to this proteomics, microfluidics, genomics, always-on sensors and high-resolution scanning and the A.I. would become the most powerful healing technology ever created, yet also the cheapest and most accessible. Communicating informationBecause so many different sources of clinical information are available, there must be an effective way of gathering them together, so that A.I. can make a fully-informed decision based on all the data. The clinical data must be communicated to the doctor, to the patient, and into databases of medical information. All doctors have some gaps in their knowledge. Their job is so complex, and they have so many things to keep track of, that they often simply forget simple things. Human error in healthcare causes hundreds of thousands of deaths. As explained in this presentation, computer programs that communicate reminders of evidence-based best practices to the point of care can overcome this problem. The ubiquity of digital communications in the modern world offers an exciting opportunity to deliver healthcare information exactly where and when it is needed. Mobile phones, social media and other digital devices can deliver the advice and guidance that a doctor would, but whereas a doctor only communicates with the patient when he is in the clinic, a mobile phone could, for example, give reminders to take pills at the right time. Artificial intelligence improves itself by studying databases, and the larger the database, the better it gets. Therefore there must be some way of collating results from large numbers of people, to optimize the A.I. systems. If high-quality healthcare is going to be made available to all human beings, information-rich medicine must therefore include a cloud computing database and clinical outcomes must be communicated to this database. This is explored further in the section on open medicine below. The results of information-rich medicineInformation-rich medicine has several noteworthy features -
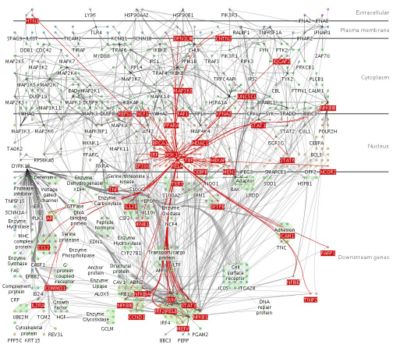 This diagram shows a small fraction of the biochemical interactions in the human brain. A doctor could not be expected to design a tailor-made intervention to nudge such a complex system into a state of health. However, artificial intelligence makes it possible to do so.
Open medicineAn information-rich medicine system will be most effective if it is open-source in three ways, which we can call open access, open data and open development. Open access here means that anyone is free to access it free of charge (as with any free website, such as YouTube). Open data means that everyone's data is added to the store, in order to improve the database for the benefit of all (as with Wikipedia). Open development means that motivated people put work into developing the tools. Open accessAll the informatics just described can (and, morally speaking, should) be free to access. Information-rich medicine is a digital product; the value is no longer in the skills of a particular physician, or in a specially-formulated molecule, but in the information. Unless there are institutional restrictions, all digital products can be free and abundant, as happened when music became digital. The cost of storing and transmitting data is tiny, compared to the costs of highly-skilled doctors with complex infrastructure, so there is really no reason medical A.I. should not be made available too all. For further discussion of open medical A.I., see these links -
Open dataRather than being stored in the private databases of a company or healthcare provider, it would be best if people's clinical data (suitably anonymized) were added to a global database. This would give the artificial intelligences more to learn from, allowing them to come to better understandings of disease. If the data is crowdsourced in this way, much more data and feedback can be gathered into the system than if data flows are restricted by secrecy and intellectual property. Compare this to the large pharmaceutical and medical companies of today, whose data is kept in-house and carefully guarded, or to paper charts kept in hospitals and referred to by only one doctor; there is no way such a system can amass anything near the same quantity of data as an open-source initiative. Mass sharing of data is possible only if free and open-source software is used; if different doctors are using different private software, their records will be incompatible, but if they are all using a common system, their records can inform one another. Where data is held privately by separate parties, the formats are incompatible and the opportunity to integrate is lost. Of 70 commercial attempts to bring Clinical Decision Support Systems Open development
Emerging treatmentsRegenerative medicineRegenerative medicine is an emerging science which aims to grow new body parts. These could either be grown in the lab and transplanted into the patient's body, or else the patient's body could be coaxed into regrowing damaged or missing parts. Your cellular machinery and genetic code was able to grow two legs already - why shouldn't it be able to grow another if you lose one in an accident? Mammalian embryos can regrow a limb if it is cut off in the first trimester of pregnancy; this is a native ability of the body, but when we age, something shuts this ability down. If we understand what this something is, we will be able to turn it off and restore the body's ability to grow organs and limbs. This will allow people suffering organ failure to have replacement organs on demand. Because their own DNA is used, their body will not attack it as foreign, as happens with transplants. Amputees could regrow their own limbs instead of using prostheses. People with spinal cord injuries could grow back their damaged nerves. Though far from complete, regenerative medicine in progressing in leaps and bounds. The key to regenerative medicine is stem cells, undifferentiated cells that can become any kind of cell. A series of breakthroughs from 2007-2009 made it possible to take adult cells and turn them into stem cells, known as Induced pluripotent stem cells 3D printing technology, using desktop printers with cells in the cartridges instead of ink, can lay down different kinds of cells in precisely-controlled patterns and build human organs. See this video for the current generation of technology. Scaffolds made of biomaterials such as collagen can be used to provide a structure onto which the cells are then applied. Similar methods applied to animal muscle could provide a less resource-intensive way of growing meat for food - see In-vitro meat. Robotic surgeryRobotic surgery is developing very rapidly. In 2000 the da Vinci robot  was the first surgical robot to be approved for market. Since then, several more sophisticated models have been developed. The coming years are sure to see major advances in this field. was the first surgical robot to be approved for market. Since then, several more sophisticated models have been developed. The coming years are sure to see major advances in this field.
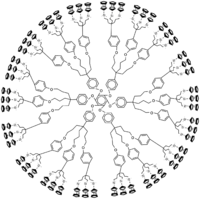
One key advantage of robotic surgery is that the movements of the surgeon's hands can be miniaturized; a surgeon can make a movement and the robotic hand can emulate the same movement, but 100 times smaller. Robotic surgery also eliminates the tiny tremors that surgeons train so hard to control, but which are an inevitable part of all fine human movement. Future generations of surgical robots will miniaturize this further, down to the micrometer level. Such robots could then even be inserted into the patient and controlled remotely from the outside. As Richard Feynman quipped in his original proposal of nanotechnology, "It would be interesting in surgery if you could swallow the surgeon." Recent progress in the areas of human-machine interface will also lead to more intuitive and precise surgical robots. For instance, a Microsoft Kinect has been modified to perform surgery [12]. The advanced scanning methods mentioned above, combined with augmented reality displays, can even be used to allow the surgeon to see inside the patient before making an incision.  The da Vinci robot is one of the first multi-purpose surgical robots to gain widespread clinical use. It can perform a wide range of operations and results in about the same clinical outcomes as conventional surgery[1]. It is the only the first generation of surgical robotics, and functions as a proof-of-concept; later versions will achieve superior results to non-robotic surgery. NanomedicineThe future may see very complex nanotechnology devices, the size of cells, that can go into the body and perform all sorts of complex tasks. See http://www.foresight.org/nanomedicine Somatic gene therapyMuch research is being done into somatic gene therapy: the attempt to change the DNA of an adult by inserting specific genes using vectors. None have yet been successful in humans, though it is common practice in mice. This could cure all genetic diseases. The fight against cancerEarly detection and preventionAs discussed above, information-rich medicine is preventive and tends to pick up diseases very early by using always-on sensors and recognizing subtle patterns. This is never more important than with cancer, where early detection makes all the difference. Researchers have built up a good idea of the environmental, genetic and other risk factors that put a person at high risk of cancer - but it is not the researchers who need to know, it is the person himself! Open-source, information-rich medicine can alert people at high risk of cancer (or, indeed, any disease), and advise them on preventive measures. For example, if your Electronic Medical Record shows you have lived near a chemical processing plant that increases risk of cancer, and you have family history of cancer, and you have a gene that is correlated with high rates of cancer, the A.I. could alert you by text message, and give you reminders to consume more anti-angiogenic foods and 'medicinal' mushrooms. When genetic screening becomes cheap enough to be commonplace, this personalized, preventive approach will be very effective. Cancer is basically a preventable disease[13], and people are more likely to comply with messages that are tailored to them than to broadcast public health campaigns, so using this method, a large fraction of cancer cases should be prevented. ProteomicsWhere cancer cannot be prevented, A.I., empowered by proteomic data, will soon be able to design systemic interventions that disrupt the molecular causes of the cancer. Rather than give people chemotherapy and hope it works, proteomic analysis will allow for a computer simulation to be built to show exactly what is happening with your biochemistry, and to simulate the effects of various interventions. These interventions may not necessarily attack the tumor itself, or even try to shrink it; as discussed above, A.I. can design interventions that work by altering the balance of biochemical system, so some of the interventions may appear unrelated to cancer; they may be such things as giving a drug that builds bone mass[14], or altering amino acid ratios in your diet. New weapons against tumorsAttacking the tumor will still remain a useful tactic, though, and we have several new and sophisticated weapons. Robotic surgery is one. Another is a kind of nanostructure known as a dendrimer, displayed to the right. Dendrimers are intricate nanoengineered molecules with beautiful snowflake-like structures. Different molecules can be attached to the surface of the structure, allowing dendrimers to act as highly customizable drug-delivery vehicles. For example, folic acid can be attached at one point on the dendrimer and an anti-cancer agent attached at another point. Because cancer cells have a hunger for folic acid, the dendrimer will be absorbed by the cancer cells, where the anti-cancer drug will kill them. This allows far lower doses to be used than if the anti-cancer agent were used alone - and more importantly, it targets only the tumor, resulting in much less toxicity to non-cancerous cells[15][16] Dendrimers can also be designed to go to the tumor site and release a florescent protein, allowing a surgeon (perhaps robot-assisted) to see exactly what tissue is and is not cancerous.A third new and elegant weapon to destroy tumors is with photodynamic therapy Tumor-treating fields are a new modality for stopping the proliferation of cancer cells. Electrodes generate electric fields tuned to the proteins that cancer cells use to divide. The force generated on the proteins inhibits their normal movement and the cells cannot divide properly. This is a very safe treatment and free of side-effects, though it is somewhat slow to work. A similar method is Irreversible Elecroporation, which punctures the membranes of cancerous cells using high-energy electric fields, leaving healthy cells untouched. "There is no medicine like hope, no incentive so great, and no tonic so powerful as expectation of something better tomorrow" - Orison Swett Marden
This page explores the application of automated information technology to healthcare, looking at how artificial intelligence can help automate healthcare and open collaboration can provide a more effective translation of knowledge into actual patient care.
The medical systems now in existence are fraught with problems. The enormous amounts of data gathered remains disconnected and scattered. Doctors are completely overwhelmed. Cancer and heart disease are on the rise in rich countries, while in poor countries infectious diseases like AIDS storm on unabated. Much research (especially pharmaceutical) is done by private companies who take decades to develop drugs, and are more interested in baldness than in malaria. An unnecessary scarcity of proper healthcare lifts it out of the reach of the poor. A single solution can simultaneously make healthcare provided to the well-off more effective and make healthcare accessible to the poor. This solution is information-rich, open medicine. By properly integrating information revolution technology into our healthcare system, we can provide, at little or no cost to the user, a healthcare system more effective than anything we have imagined. We can switch from a system where medical treatment depends on scarce expertise and drugs to a system where it depends on ubiquitous information. Information-rich medicineThere are three elements in an information-rich medical system, all of which are greatly empowered by information technology: information must be gathered, processed, and communicated. These are explored in greater detail below. There are compelling reasons for setting up this information infrastructure according to open-source principles, where the platform and its content are built collaboratively, rather than being in the hands of a particular institution. Gathering informationWe have new, exponentially accelerating, ways of gathering medical and biological information. Traditionally, a doctor made clinical decisions based on the patient's descriptions of their symptoms and perhaps a few tests or low-resolution scans. But the body is a very complex thing, and this information gives only a very grainy picture of what is really happening. Several recently developed technologies allow us to gather literally millions of times more information about what's really going on in the body than was possible a few years ago -
These are the enabling tools of information-rich medicine. Using them in concert, you can build up a highly-detailed computerized set of information about what is going on with your body. Of course, to use the data effectively, it must be processed. Processing informationThis river of raw data would do a doctor no good; it would simply be overwhelming. This is where the pattern-recognition abilities of artificial intelligence are required. In the same way that artificial intelligence can recognize patterns showing a coming upswing in a stock market, it can recognize patterns in a heart rhythm indicating a coming heart attack. By applying A.I. to the data generated, we can turn raw data into clinically-relevant knowledge. This is already common practice in hospitals, where A.I. is routinely used for tasks like analyzing electrocardiograms. But can modern artificial intelligence really diagnose disease as effectively as human doctors? The surprising answer is that even mid-1970s artificial intelligence could. In the 1970s, an A.I. called MYCIN proved itself able to perform medical diagnosis as well as, or better than, human doctors. A patient can even do much of this processing on his or her smartphone. Smartphones can do blood glucose analysis, reconstruct ultrasound images and read and diagnose ECGs. Tasks demanding more computing power will require distributed cloud computing. One application of this is rational drug design, where A.I. considers the molecular basis of disease and computes the exact molecular intervention that is needed. This is a vast improvement on the old way of designing drugs based on chemical families. Even if the sophisticated information-gathering methods just described are not fully exploited, using existing artificial intelligence to process clinical information can greatly improve clinical outcomes. Imagine for a moment that if you walk into a clinic, modern information technologies whirr into action and pull from a distributed global network your medical record and family history. You describe your symptoms to the doctor, who inputs them into a handheld computer. The computer processes the symptoms and cross-references them with a database of known diseases. It compares all similarly-presenting cases – no matter where in the world those other cases happened. It uses all this information to create a list of possible diagnoses, then uses optimized and self-improving artificial intelligence algorithms to calculate the likelihood of each one, based on your medical history, race, age, sex and so forth. The computer displays a list of possible conditions and possible courses of action, including treatments or further testing. If a scan is done, say an X-ray, the computer can identify patterns in it and use this to inform its diagnosis. Such a system would never overlook a piece of data such as a drug interaction or allergy, and could intelligently update itself based on the entirety of mankind's medical knowledge. Add to this proteomics, microfluidics, genomics, always-on sensors and high-resolution scanning and the A.I. would become the most powerful healing technology ever created, yet also the cheapest and most accessible. Communicating informationBecause so many different sources of clinical information are available, there must be an effective way of gathering them together, so that A.I. can make a fully-informed decision based on all the data. The clinical data must be communicated to the doctor, to the patient, and into databases of medical information. All doctors have some gaps in their knowledge. Their job is so complex, and they have so many things to keep track of, that they often simply forget simple things. Human error in healthcare causes hundreds of thousands of deaths. As explained in this presentation, computer programs that communicate reminders of evidence-based best practices to the point of care can overcome this problem. The ubiquity of digital communications in the modern world offers an exciting opportunity to deliver healthcare information exactly where and when it is needed. Mobile phones, social media and other digital devices can deliver the advice and guidance that a doctor would, but whereas a doctor only communicates with the patient when he is in the clinic, a mobile phone could, for example, give reminders to take pills at the right time. Artificial intelligence improves itself by studying databases, and the larger the database, the better it gets. Therefore there must be some way of collating results from large numbers of people, to optimize the A.I. systems. If high-quality healthcare is going to be made available to all human beings, information-rich medicine must therefore include a cloud computing database and clinical outcomes must be communicated to this database. This is explored further in the section on open medicine below. The results of information-rich medicineInformation-rich medicine has several noteworthy features -
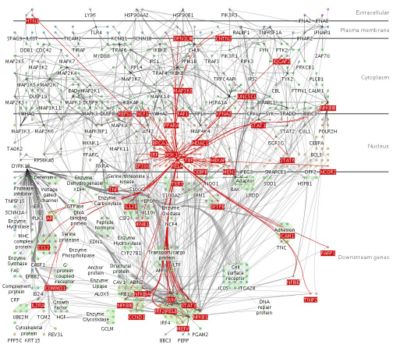 This diagram shows a small fraction of the biochemical interactions in the human brain. A doctor could not be expected to design a tailor-made intervention to nudge such a complex system into a state of health. However, artificial intelligence makes it possible to do so.
Open medicineAn information-rich medicine system will be most effective if it is open-source in three ways, which we can call open access, open data and open development. Open access here means that anyone is free to access it free of charge (as with any free website, such as YouTube). Open data means that everyone's data is added to the store, in order to improve the database for the benefit of all (as with Wikipedia). Open development means that motivated people put work into developing the tools. Open accessAll the informatics just described can (and, morally speaking, should) be free to access. Information-rich medicine is a digital product; the value is no longer in the skills of a particular physician, or in a specially-formulated molecule, but in the information. Unless there are institutional restrictions, all digital products can be free and abundant, as happened when music became digital. The cost of storing and transmitting data is tiny, compared to the costs of highly-skilled doctors with complex infrastructure, so there is really no reason medical A.I. should not be made available too all. For further discussion of open medical A.I., see these links -
Open dataRather than being stored in the private databases of a company or healthcare provider, it would be best if people's clinical data (suitably anonymized) were added to a global database. This would give the artificial intelligences more to learn from, allowing them to come to better understandings of disease. If the data is crowdsourced in this way, much more data and feedback can be gathered into the system than if data flows are restricted by secrecy and intellectual property. Compare this to the large pharmaceutical and medical companies of today, whose data is kept in-house and carefully guarded, or to paper charts kept in hospitals and referred to by only one doctor; there is no way such a system can amass anything near the same quantity of data as an open-source initiative. Mass sharing of data is possible only if free and open-source software is used; if different doctors are using different private software, their records will be incompatible, but if they are all using a common system, their records can inform one another. Where data is held privately by separate parties, the formats are incompatible and the opportunity to integrate is lost. Of 70 commercial attempts to bring Clinical Decision Support Systems Open development
Emerging treatmentsRegenerative medicineRegenerative medicine is an emerging science which aims to grow new body parts. These could either be grown in the lab and transplanted into the patient's body, or else the patient's body could be coaxed into regrowing damaged or missing parts. Your cellular machinery and genetic code was able to grow two legs already - why shouldn't it be able to grow another if you lose one in an accident? Mammalian embryos can regrow a limb if it is cut off in the first trimester of pregnancy; this is a native ability of the body, but when we age, something shuts this ability down. If we understand what this something is, we will be able to turn it off and restore the body's ability to grow organs and limbs. This will allow people suffering organ failure to have replacement organs on demand. Because their own DNA is used, their body will not attack it as foreign, as happens with transplants. Amputees could regrow their own limbs instead of using prostheses. People with spinal cord injuries could grow back their damaged nerves. Though far from complete, regenerative medicine in progressing in leaps and bounds. The key to regenerative medicine is stem cells, undifferentiated cells that can become any kind of cell. A series of breakthroughs from 2007-2009 made it possible to take adult cells and turn them into stem cells, known as Induced pluripotent stem cells 3D printing technology, using desktop printers with cells in the cartridges instead of ink, can lay down different kinds of cells in precisely-controlled patterns and build human organs. See this video for the current generation of technology. Scaffolds made of biomaterials such as collagen can be used to provide a structure onto which the cells are then applied. Similar methods applied to animal muscle could provide a less resource-intensive way of growing meat for food - see In-vitro meat. Robotic surgeryRobotic surgery is developing very rapidly. In 2000 the da Vinci robot  was the first surgical robot to be approved for market. Since then, several more sophisticated models have been developed. The coming years are sure to see major advances in this field. was the first surgical robot to be approved for market. Since then, several more sophisticated models have been developed. The coming years are sure to see major advances in this field.
One key advantage of robotic surgery is that the movements of the surgeon's hands can be miniaturized; a surgeon can make a movement and the robotic hand can emulate the same movement, but 100 times smaller. Robotic surgery also eliminates the tiny tremors that surgeons train so hard to control, but which are an inevitable part of all fine human movement. Future generations of surgical robots will miniaturize this further, down to the micrometer level. Such robots could then even be inserted into the patient and controlled remotely from the outside. As Richard Feynman quipped in his original proposal of nanotechnology, "It would be interesting in surgery if you could swallow the surgeon." Recent progress in the areas of human-machine interface will also lead to more intuitive and precise surgical robots. For instance, a Microsoft Kinect has been modified to perform surgery [26]. The advanced scanning methods mentioned above, combined with augmented reality displays, can even be used to allow the surgeon to see inside the patient before making an incision.  The da Vinci robot is one of the first multi-purpose surgical robots to gain widespread clinical use. It can perform a wide range of operations and results in about the same clinical outcomes as conventional surgery[2]. It is the only the first generation of surgical robotics, and functions as a proof-of-concept; later versions will achieve superior results to non-robotic surgery. NanomedicineThe future may see very complex nanotechnology devices, the size of cells, that can go into the body and perform all sorts of complex tasks. See http://www.foresight.org/nanomedicine Somatic gene therapyMuch research is being done into somatic gene therapy: the attempt to change the DNA of an adult by inserting specific genes using vectors. None have yet been successful in humans, though it is common practice in mice. This could cure all genetic diseases. The fight against cancerEarly detection and preventionAs discussed above, information-rich medicine is preventive and tends to pick up diseases very early by using always-on sensors and recognizing subtle patterns. This is never more important than with cancer, where early detection makes all the difference. Researchers have built up a good idea of the environmental, genetic and other risk factors that put a person at high risk of cancer - but it is not the researchers who need to know, it is the person himself! Open-source, information-rich medicine can alert people at high risk of cancer (or, indeed, any disease), and advise them on preventive measures. For example, if your Electronic Medical Record shows you have lived near a chemical processing plant that increases risk of cancer, and you have family history of cancer, and you have a gene that is correlated with high rates of cancer, the A.I. could alert you by text message, and give you reminders to consume more anti-angiogenic foods and 'medicinal' mushrooms. When genetic screening becomes cheap enough to be commonplace, this personalized, preventive approach will be very effective. Cancer is basically a preventable disease[27], and people are more likely to comply with messages that are tailored to them than to broadcast public health campaigns, so using this method, a large fraction of cancer cases should be prevented. ProteomicsWhere cancer cannot be prevented, A.I., empowered by proteomic data, will soon be able to design systemic interventions that disrupt the molecular causes of the cancer. Rather than give people chemotherapy and hope it works, proteomic analysis will allow for a computer simulation to be built to show exactly what is happening with your biochemistry, and to simulate the effects of various interventions. These interventions may not necessarily attack the tumor itself, or even try to shrink it; as discussed above, A.I. can design interventions that work by altering the balance of biochemical system, so some of the interventions may appear unrelated to cancer; they may be such things as giving a drug that builds bone mass[28], or altering amino acid ratios in your diet. New weapons against tumorsAttacking the tumor will still remain a useful tactic, though, and we have several new and sophisticated weapons. Robotic surgery is one. Another is a kind of nanostructure known as a dendrimer, displayed to the right. Dendrimers are intricate nanoengineered molecules with beautiful snowflake-like structures. Different molecules can be attached to the surface of the structure, allowing dendrimers to act as highly customizable drug-delivery vehicles. For example, folic acid can be attached at one point on the dendrimer and an anti-cancer agent attached at another point. Because cancer cells have a hunger for folic acid, the dendrimer will be absorbed by the cancer cells, where the anti-cancer drug will kill them. This allows far lower doses to be used than if the anti-cancer agent were used alone - and more importantly, it targets only the tumor, resulting in much less toxicity to non-cancerous cells[29][30] Dendrimers can also be designed to go to the tumor site and release a florescent protein, allowing a surgeon (perhaps robot-assisted) to see exactly what tissue is and is not cancerous.A third new and elegant weapon to destroy tumors is with photodynamic therapy Tumor-treating fields are a new modality for stopping the proliferation of cancer cells. Electrodes generate electric fields tuned to the proteins that cancer cells use to divide. The force generated on the proteins inhibits their normal movement and the cells cannot divide properly. This is a very safe treatment and free of side-effects, though it is somewhat slow to work. A similar method is Irreversible Elecroporation, which punctures the membranes of cancerous cells using high-energy electric fields, leaving healthy cells untouched. |
 [print version]
[print version]  [update]
[update]  [site map]
[site map]